June 22, 2017
You asked, and we listened. MIE wants to put your minds at rest on MACRA, the Quality Payment Program (QPP), and any potential penalties that may be delivered in calendar year (CY) 2019, under MIPS. As you may know, CMS puts out a great deal of information, and sometimes that information can be difficult to navigate. The last thing you need is more to worry about, so let us address your concerns as concisely and simply as possible and give back a little more time to your day.
The introductory year of the QPP has been formulated as a Transition Year (TY 2017), with a Pick-Your-Pace design, for MIPS participants. The performance threshold has been lowered in such a way that minimal participation can avoid a downward adjustment in CY 2019. Here is what you need to do:
As of June 21st, CMS announced their intention to streamline and reduce clinician burden while participating in the QPP, for CY 2018. The goal is to continue into next year using what works, modifying the QPP requirements, based on stakeholder feedback. There are several proposed items to consider. For example:
Take a moment and review the Proposed Rule for Quality Payment Program Year 2, which is currently in its 60-day comment period, until August 18th. MIE will continue to follow this Proposed Rule and review the Final Rule, when it comes available.
For this year, there are four paths under the Pick-Your-Pace design that MIE classifies as the following actions: 1) Do Nothing, 2) Avoid the Penalty, 3) Build Momentum, and 4) Excel. Below, there is a brief explanation of the associated expectations of each pace and their anticipated adjustment potential, followed by a table of attestation requirements for each MIPS category, as they relate to the given track.

This is the most basic and easiest path to understand; do nothing while eligible, and CY 2019 will come with a negative four percent (-4%) downward payment adjustment.
For eligible clinicians, this path provides the easiest means to assure no penalty will be incurred for CY 2019. Each of the three categories (Quality, Advancing Care Information, and Improvement Activities) calculated for the TY 2017 Final Score have minimum requirements, which when met, guarantee a neutral adjustment, minimally.
| Category | Quality | ACI | IA |
|---|---|---|---|
| Requirements | One (1) Quality Measure | Four (4) Required Measures of Base Score* | One (1) Improvement Activity (High or Med) |
*The required Advancing Care Information Base Score measure set is determined by the electronic health record (EHR) edition being used. In addition to the Base Score, Partial and Full Participation paces track additional measures under the Performance and Bonus Scores, for a potential maximum adjustment. For more information regarding EHR editions and ACI measure sets, see the Quality Payment Program (QPP) Advancing Care Information webpage and Fact Sheet.
This progressive pace is oriented around a 90-day reporting period. Its appeal comes from its natural way of building momentum through the impetus created from a successful approach to and understanding of quality care. Though the reporting requirements increase under this pace, the 90-day reporting period allows for a familiarization with the attestation requirements, scoring methodology, and incentivization. Clinicians have the ability to earn the maximum adjustment with this track, based on the quality of the data submitted. Ultimately, this path will always produce a neutral or positive payment adjustment, when executed effectively.
| Category | Quality | ACI | IA |
|---|---|---|---|
| Requirements | Six (6) Quality Measures (including 1 Outcome Measure)* | Base Score + add’l measures to increase Performance Score | 2 High or 1 High & 2 Med or 4+ Med |
*Partial and Full Participation paces require no fewer than six (6) Quality Measures, of which, one (1) is required to be an Outcome Measure. However, specialty-specific measure sets are available for qualifying clinicians, and may be reviewed on the QPP Quality Measures webpage.
This more aggressive pace requires full participation and is excellent for the clinician prepared to show their ability to excel at patient care and quality reporting. This track adheres to a full-year reporting period and guarantees a modest to moderate positive payment adjustment, based on the quality of data supplied.
| Category | Quality | ACI | IA |
|---|---|---|---|
| Requirements | Six (6) Quality Measures (including 1 Outcome Measure) | Base Score + add’l measures to increase Performance Score | 2 High or 1 High & 2 Med or 4+ Med* |
*The Partial and Full Participation paces account for most participants; however, there are accommodations built into the scoring for groups of 15 or fewer clinicians and/or clinicians working as non-patient facing or within a rural area. For more information see the CMS Improvement Activities Fact Sheet.
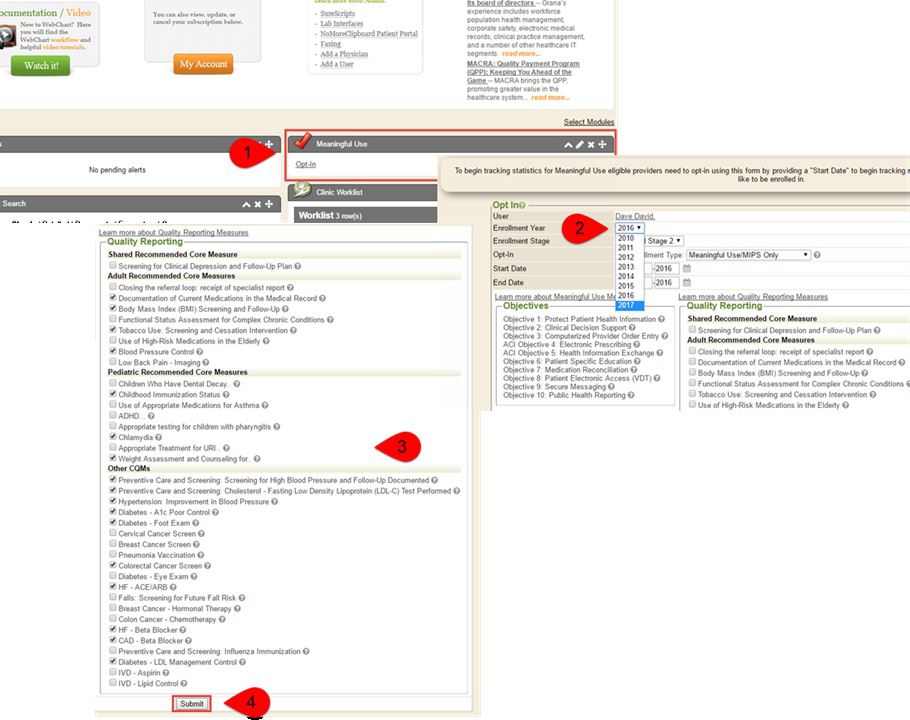
If you are eligible and planning to get ahead of the game, opt into MIPS, now! Keep in mind that HIPAA requirements, as well as the Advancing Care Information category, call for eligible clinicians to provide a Security Risk Analysis, as a standard for CEHRT use. To be successful, simply perform your Security Risk Analysis, follow these easy steps, and MIE will do the rest:
If you have questions, or you are still unclear about MIPS and its requirements, review the MIPS Fact Sheet, or send us your questions. If you would rather, call us with your concerns. MIE Helpdesk is available 24 hours a day, every day, and can be reached via email at support@mieweb.com, or, by telephone at (260) 459-6270, Option 1, or toll free 1-888-498-3484, Option 1.